Understanding Osteoporosis and Osteoporotic Fractures
Osteoporosis is a common condition that weakens bones, making them fragile and more prone to fractures. It’s often referred to as a “silent disease” because bone loss occurs without symptoms. The first sign might be a fracture due to a minor fall or, in severe cases, even from sneezing or coughing.
What is Osteoporosis?
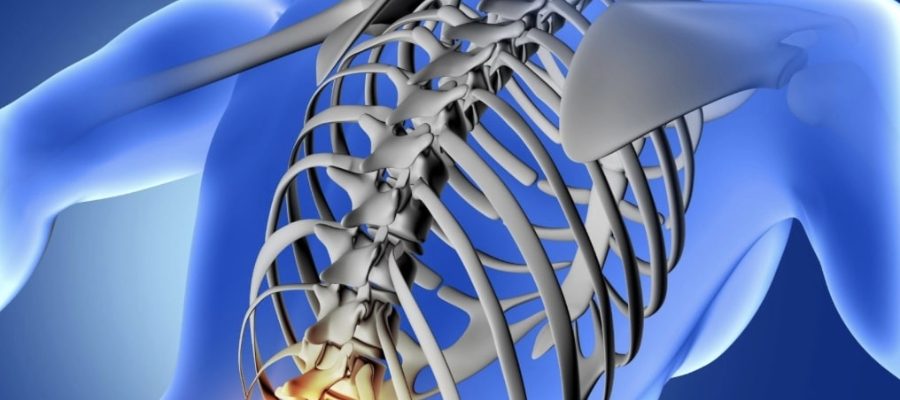
Osteoporosis is a condition characterized by a decrease in bone density and strength, leading to an increased risk of fractures, known as osteoporotic fractures. These fractures most commonly occur in the hip, spine, and wrist, but can affect any bone.
How Osteoporosis Can Cause Osteoporotic Fractures?
Osteoporotic fractures are a direct result of the reduced bone density caused by osteoporosis. The spine is particularly vulnerable; vertebral fractures can lead to significant pain, loss of height, and spinal deformities.
Commonly Affected Bones in Osteoporosis
Osteoporosis can affect any bone in the body, but certain bones are more susceptible to fractures due to their structure and function. The most commonly affected bones in individuals with osteoporosis are:
Hip Bones:
Hip fractures are particularly serious and often require surgical intervention. They can lead to loss of independence and are sometimes life-threatening in older adults.
Wrist (Distal Radius)
Wrist fractures are common, especially in postmenopausal women. Such fractures typically occur from a fall onto an outstretched hand.
Spine (Vertebrae):
Vertebral fractures can occur with minimal trauma. These can cause severe pain, kyphosis (a forward curvature of the spine), and significant reductions in height.
Rib Bones:
Rib fractures can result from minor trauma or even severe coughing, leading to significant discomfort and impaired movement.
This helps in the prevention, early detection, and management of osteoporosis to mitigate the risk of fractures.
Causes of Osteoporosis
Several factors can contribute to the development of osteoporosis, including:
Hormonal Changes
A decline in estrogen levels in women during menopause or testosterone in men can lead to bone loss.
Dietary Factors
Insufficient calcium or vitamin D intake can weaken bones.
Lifestyle Choices
Lack of physical activity, smoking, and excessive alcohol consumption can increase the risk.
Medical Conditions
Certain conditions like rheumatoid arthritis or chronic kidney disease can contribute to bone loss.
Symptoms of Osteoporosis
Often, there are no symptoms until a fracture occurs. However, warning signs may include:
Back pain
Loss of height over time
A stooped posture
Bones that break more easily than expected
Diagnosing Osteoporosis
It is typically diagnosed through a bone density test, known as a DEXA scan. This test measures the density of bones in various parts of the body and helps determine the risk of fractures.
Steps to Diagnose Osteoporosis
1. Evaluate Risk Factors
At Total Orthopaedic, we will begin the evaluation of risk factors, review your medical history, lifestyle, and family history to assess your likelihood of developing osteoporosis.
Key risk factors include:
- Advanced age
- Gender (women, particularly postmenopausal, are at higher risk)
- Previous fractures
- Family history of osteoporosis
- Smoking or excessive alcohol use
- Low calcium or vitamin D intake
- Sedentary lifestyle
Advanced age
Gender (women, particularly postmenopausal, are at higher risk)
Previous fractures
Family history of osteoporosis
Smoking or excessive alcohol use
Low calcium or vitamin D intake
Sedentary lifestyl
2. Physical Examination
The next step is a physical exam to identify any signs of bone density loss. Our Osteoporosis specialist might look for:
A decrease in height or posture changes, which can indicate compression fractures
Pain in the spine or hips
3. Bone Density Tests (DXA or DEXA Scan)
A Dual-Energy X-ray Absorptiometry (DXA) scan is the most common and accurate test for diagnosing osteoporosis. It measures bone mineral density (BMD), usually in the spine, hip, or wrist.
How it Works:
The scan uses low-dose X-rays to create detailed images of your bones. The results are compared to the bone density of a healthy young adult (T-score) and someone your age and sex (Z-score).
Interpreting Results:
- Normal bone density: T-score of -1.0 or above
- Low bone density (osteopenia): T-score between -1.0 and -2.5
- Osteoporosis: T-score of -2.5 or lower
4. X-rays and Imaging Tests
X-rays are sometimes used but are less effective in detecting early bone loss. They might be performed to evaluate fractures, deformities, or structural problems caused by osteoporosis.
5. Blood and Urine Tests
To rule out other conditions or identify potential causes of bone loss, your doctor may recommend lab tests such as:
- Calcium and Vitamin D Levels: To ensure your body has adequate nutrients for bone health
- Thyroid Function Tests: Overactive thyroid can weaken bones
- Bone Turnover Markers: These may help track how quickly your bone is being broken down and rebuilt
6. FRAX® Assessment
FRAX® (Fracture Risk Assessment Tool) is often used alongside a DXA scan. It estimates your 10-year probability of experiencing a major osteoporotic fracture based on risk factors and BMD results.
When to Get Tested
You should consider a bone density test or speak with your doctor about screening if you are:
A postmenopausal woman
Over 50 and have experienced a fracture
A man over 70 or a woman over 65
Younger but with known risk factors (such as family history or medication use like corticosteroids)
Treating Osteoporotic Fractures at Total Orthopaedic
Fractures can significantly impair quality of life and often require a combination of medical and surgical care. For osteoporotic fracture treatment our doctors will recommend will do the following:
Non-Surgical Interventions:
- Bracing: Spinal braces can provide support for vertebral fractures, reducing pain during recovery.
- Rehabilitation: Physical therapy is crucial for regaining strength, balance, and function after a fracture.
Surgical Interventions:
For severe fractures or when conservative treatments fail, surgery may be necessary:
- Vertebroplasty/Kyphoplasty: Cement-like material is injected into fractured vertebrae to stabilize and reduce pain.
- Joint Replacement: Hip fractures often require partial or total hip replacement surgery.
- Open Reduction and Internal Fixation (ORIF): For complex fractures, hardware like screws and plates may be used to stabilize the bone.
Osteoporotic Fracture Pain Management:
Over-the-counter or prescription pain relievers help manage acute pain after a fracture.
Physical therapy may alleviate pain and improve mobility over time.
Other Treatment Options for Osteoporosis
While osteoporosis can’t be completely cured, several treatments can help manage the condition and strengthen bones:
Lifestyle Changes
A diet rich in calcium and vitamin D, regular weight-bearing exercises, quitting smoking, and reducing alcohol intake.
Medications
Medications are a key aspect of osteoporosis treatment, aimed at slowing bone loss or stimulating bone formation. We determine the appropriate medication based on bone density test results, fracture history, and individual risk factors.
Bisphosphonates (e.g., alendronate, risedronate) help prevent bone loss.
Calcitonin and denosumab, which help regulate bone metabolism and prevent bone resorption.
Selective Estrogen Receptor Modulators (SERMs)
It mimic estrogen's bone-preserving effects.
Calcitonin and denosumab, which help regulate bone metabolism and prevent bone resorption.
Why Choose Us?
If you’re experiencing symptoms of osteoporosis or are concerned about your bone health, it’s crucial to consult with a spine specialist. We can provide personalised advice and treatment options tailored to your needs. Early detection and appropriate management can significantly improve quality of life and reduce the risk of osteoporotic fractures. Don’t wait—safeguard your spine health today.



